Comprehensive Overview of Drainage Bags: Usage, Safety, and Innovations
Drainage bags are critical medical devices used to collect bodily fluids in a safe, sterile, and controlled manner. Their use spans a range of clinical scenarios, from urinary catheterization to post-operative wound drainage and specialized fluid management in chest or abdominal procedures. These bags are integral to both acute inpatient care and long-term management in nursing homes or home-care settings, providing effective fluid removal, facilitating monitoring, and helping reduce the risk of infection or complications.
The most widespread application of drainage bags is in conjunction with indwelling urinary catheters. These systems allow continuous urine drainage from the bladder when a patient is unable to void naturally—common in surgical recovery, neurogenic bladder conditions, or severe mobility impairments. In surgical settings, drainage bags are often connected to negative-pressure or gravity drains that remove blood, pus, or serous fluid from the operative site. Removing this fluid reduces local pressure, promotes healing, and lowers the risk of fluid collections such as hematomas or abscesses. In all cases, proper positioning of the drainage bag—typically below the insertion site—is essential to ensure gravity-dependent flow and prevent retrograde contamination.
A typical drainage bag system consists of several interconnected components, each playing a vital role in performance and safety. The primary element is the collection reservoir, whose capacity varies depending on the intended use. Leg bags, used for ambulatory patients, generally range from 300 to 600 mL, while bedside or overnight bags can hold up to 2,000 mL. The bag is connected to the body via flexible medical-grade tubing, which is attached to a catheter or surgical drain. This tubing must provide a secure, leak-proof, and sterile conduit for fluid transfer.
At the bottom of the bag is the drainage outlet, often a twist valve, flip valve, or slide-tap mechanism, which allows caregivers to empty the contents without disconnecting the system. Most modern bags also incorporate an anti-reflux valve, which prevents backward flow of fluid—a critical infection control feature. Graduated measurement markings along the side of the reservoir enable precise fluid output monitoring, which is essential for managing patient hydration status, identifying signs of infection, or adjusting therapy. Additional components may include hanger hooks for bedside mounting or adjustable straps for securing leg bags to the thigh or calf.

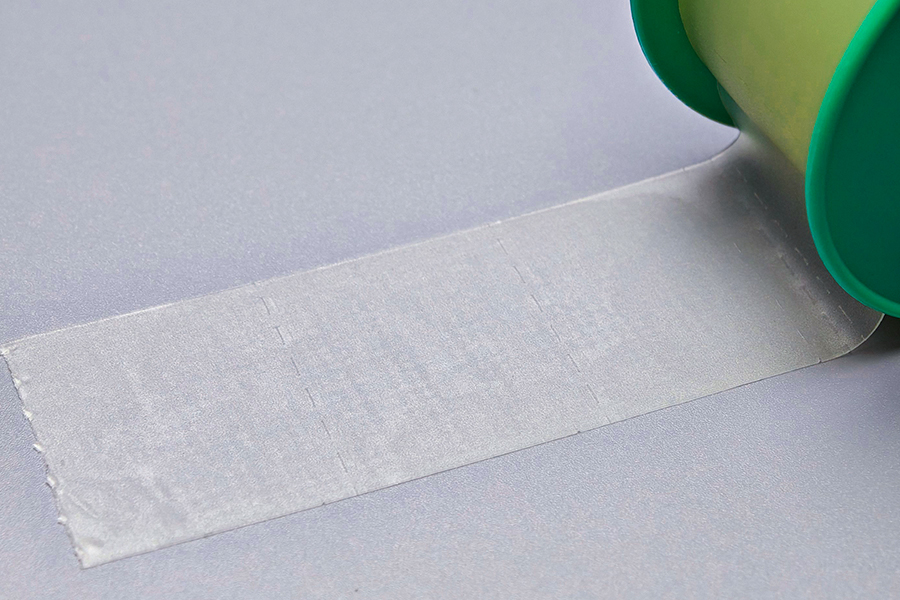
The materials used in the manufacturing of drainage bags must meet strict standards for biocompatibility, durability, and sterility. The most commonly used material is medical-grade polyvinyl chloride (PVC) due to its clarity, flexibility, and cost-effectiveness. PVC is latex-free, which reduces the risk of allergic reactions, and is durable enough to maintain structural integrity even when filled to capacity. In applications requiring softer or more biocompatible materials—such as long-term indwelling components—silicone or polyurethane may be used, particularly for tubing or catheter interfaces. Some advanced drainage systems may feature multilayer film structures that combine polyethylene for leak resistance with polyurethane for tensile strength.
Infection control is one of the most critical considerations in the use of drainage bags. All components are typically sterilized during production and packaged in sealed, contamination-proof conditions. Many systems are intended for single use, particularly in surgical or catheter-associated scenarios, to minimize the risk of healthcare-associated infections (HAIs). For devices used over several days, strict protocols govern replacement intervals, cleaning of ports, and maintenance of closed-system integrity. Innovations such as antimicrobial-coated tubing, needle-free sampling ports, and one-way valves have further enhanced safety in recent years.
For patients managing drainage systems at home—particularly those with chronic catheter use or post-operative drains—proper education is essential. Patients and caregivers must understand how to empty and clean the bag, recognize signs of infection (such as cloudy or foul-smelling output, fever, or erythema at the insertion site), and know when to seek medical attention. Inappropriate handling can result in ascending infections or mechanical failure of the device. Therefore, easy-to-use designs, discreet leg bags for mobility, and accessible instructions are increasingly prioritized in product development.
In summary, drainage bags are a foundational component of modern medical care, enabling efficient fluid management, reducing infection risk, and supporting clinical decision-making. Their design reflects a balance of practicality, hygiene, and patient comfort. As healthcare shifts increasingly toward outpatient and home-based care, the role of user-friendly, high-quality drainage bag systems will only continue to grow—making them not only a clinical necessity but a central part of long-term care infrastructure.

 English
English Français
Français Español
Español Português
Português عربى
عربى