Sterile vs Non-Sterile Medical Products: Selection Guide
The distinction between sterile and non-sterile medical products represents one of the most critical decisions in healthcare procurement. After two decades of manufacturing medical disposables, we've witnessed how this single choice affects patient outcomes, cost efficiency, and regulatory compliance across hospitals worldwide. The decision isn't always straightforward—even products that seem identical may require different sterility levels depending on their intended use.
Understanding when to select sterile versus non-sterile products requires knowledge of infection control principles, regulatory requirements, and practical application contexts. This guide draws from our manufacturing experience and feedback from healthcare facilities across Europe, Africa, the Middle East, and the Americas to help you make informed procurement decisions.
Understanding Sterility Standards and Classifications
Sterile medical products must meet a Sterility Assurance Level (SAL) of 10⁻⁶, meaning there is less than one-in-a-million chance of a viable microorganism remaining on the product. This is achieved through validated sterilization methods including ethylene oxide (EtO) gas, gamma radiation, or steam autoclaving. Each method has specific applications—EtO works well for heat-sensitive materials like certain gauzes and catheters, while gamma radiation is preferred for pre-packaged items in their final containers.
Non-sterile products, conversely, are manufactured under controlled conditions but without terminal sterilization. They typically carry a bioburden level below 100 colony-forming units (CFU) per product, suitable for applications where the product won't contact compromised tissue or enter sterile body cavities. The manufacturing environment for non-sterile items maintains cleanliness standards but doesn't require the stringent environmental controls of sterile production lines.
Regulatory Framework Differences
Regulatory bodies classify medical devices based on risk levels, which directly influences sterility requirements. In the EU MDR system, Class I sterile devices require notified body involvement, while non-sterile Class I devices can often self-certify. The FDA similarly distinguishes between devices requiring sterility (typically Class II and III) and those that don't. From our production facility in Suzhou, we maintain separate manufacturing areas and quality systems for sterile and non-sterile products to meet these distinct regulatory pathways. Our complete product range includes both sterile and non-sterile options across multiple device categories, manufactured according to ISO 13485 standards with appropriate sterility validations where required.
Critical Applications Requiring Sterile Products
Certain medical applications categorically demand sterile products, regardless of cost considerations. The risk of infection in these contexts is simply too high to accept any microbial contamination.
Surgical and Invasive Procedures
Any product entering a sterile body cavity or contacting normally sterile tissue must be sterile. This includes surgical gauze swabs, lap sponges used in open surgeries, and surgical drapes that create the sterile field. During a typical appendectomy, for instance, every gauze swab used to control bleeding must be sterile—a single contaminated swab can introduce pathogens directly into the peritoneal cavity, potentially causing life-threatening peritonitis.
We've observed infection rate reductions of 40-60% in surgical departments that transitioned from attempting to sterilize non-sterile gauze in-house to using factory-sterilized products. Hospital sterilization departments, while capable, often face workload pressures that can compromise sterilization cycle validation and quality control.
Catheterization and Urological Procedures
Urinary catheters entering the bladder must be sterile to prevent catheter-associated urinary tract infections (CAUTIs), which affect 15-25% of hospitalized patients with catheters according to CDC data. Both Foley catheters for long-term use and Nelaton catheters for intermittent catheterization require sterility. The urinary tract, though not completely sterile, becomes highly susceptible to infection when a foreign body is introduced.
Wound Care for Compromised Skin Integrity
Open wounds, burns covering more than 20% total body surface area, and chronic ulcers with exposed subcutaneous tissue require sterile dressings. The skin's barrier function is compromised, making these wounds portals for systemic infection. Sterile paraffin gauze for burns, sterile alginate dressings for exuding wounds, and sterile surgical pads for post-operative wounds all serve to protect while healing occurs.
Appropriate Applications for Non-Sterile Products
Many clinical applications perform equally well with non-sterile products, offering significant cost savings without compromising patient safety. Understanding these applications prevents unnecessary expenditure on sterility when it provides no clinical benefit.
Intact Skin Applications
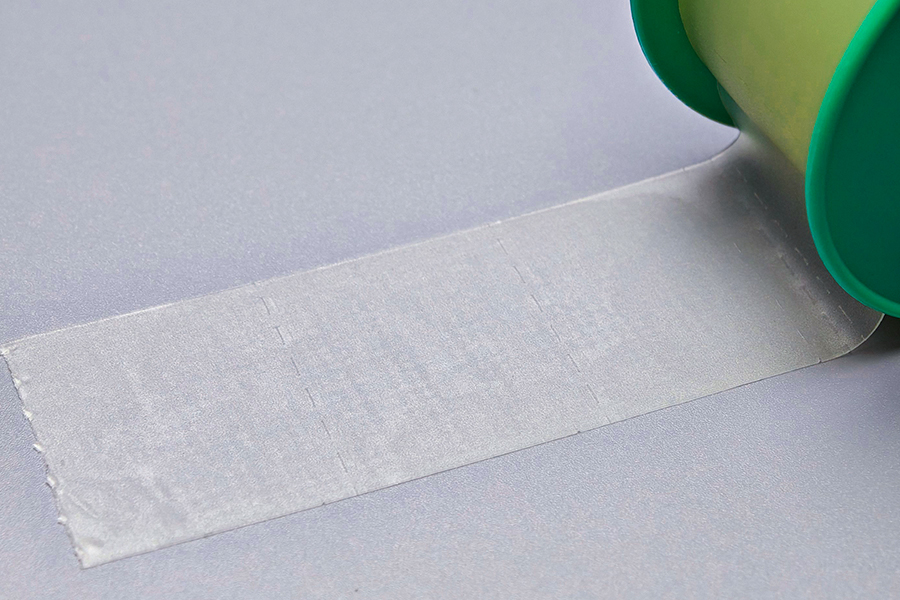
Products contacting intact skin rarely require sterility. Bandages securing IV sites, elastic bandages for sprains, medical tapes for dressing retention, and compression bandages all function perfectly well in non-sterile form. The skin itself harbors millions of bacteria per square centimeter—adding sterile products to intact skin provides no infection control advantage. We estimate that hospitals using non-sterile elastic bandages instead of sterile alternatives save approximately $0.80-$1.20 per application with identical clinical outcomes.
Examination and Diagnostic Procedures
Non-sterile examination gloves are appropriate for patient examination, venipuncture, and handling contaminated materials. Only surgical gloves entering sterile fields require sterility. Cotton swabs for specimen collection from non-sterile sites (throat, nasal, wound surface cultures) don't require sterility—though the transport medium should be sterile to preserve the specimen. Tongue depressors, measuring tapes, and examination table paper all perform their functions without sterilization.
Minor Wound Care and First Aid
Superficial cuts, abrasions, and minor burns with intact epidermis can be managed with non-sterile gauze, cotton balls, and adhesive bandages. The wound cleaning process (irrigation and antiseptic application) reduces bioburden more significantly than the sterility status of the covering material. For emergency departments and first aid stations managing high volumes of minor injuries, non-sterile supplies offer practical efficiency. One emergency department we supply reported treating 300+ minor wounds monthly exclusively with non-sterile gauze and adhesive strips without any infection complications.
Cost Analysis: Sterile versus Non-Sterile Economics
The price differential between sterile and non-sterile products varies by product type, but generally ranges from 150% to 400% higher for sterile versions. This cost difference stems from sterilization processing, validation testing, sterile packaging materials, and more stringent quality control requirements.
| Product Type | Non-Sterile Cost | Sterile Cost | Price Increase |
|---|---|---|---|
| Gauze Swab 10×10cm | $0.02 | $0.08 | 300% |
| Elastic Bandage 10cm×4.5m | $0.45 | $1.15 | 156% |
| Examination Gloves (pair) | $0.08 | $0.32 | 300% |
| Cotton Balls (100pc pack) | $0.75 | $2.25 | 200% |
For a 300-bed hospital, inappropriate use of sterile products where non-sterile would suffice can waste $75,000-$150,000 annually. Conversely, using non-sterile products in applications requiring sterility can lead to surgical site infections costing an average of $20,000 per infection in extended hospitalization and treatment.
Hidden Costs Beyond Purchase Price
Beyond unit cost, consider storage requirements—sterile products require specific environmental controls to maintain package integrity. Humidity above 70% or storage temperatures exceeding 25°C can compromise sterile barrier systems. Expiration management becomes more critical with sterile inventory, as typical shelf life is 3-5 years compared to longer periods for non-sterile items. Staff training on sterile technique, though necessary, also represents an ongoing cost for facilities handling sterile supplies.
Decision Framework: Selecting the Right Sterility Level
We've developed a practical decision framework based on thousands of customer consultations to help healthcare buyers make appropriate sterility choices:
Risk Assessment Questions
- Will the product contact normally sterile tissue or body cavities? If yes, sterile is mandatory. This includes products for surgery, catheterization, and injection.
- Does the patient have compromised immunity or barrier defenses? Neutropenic patients, burn victims, and those with extensive wounds may require sterile products even for applications that would typically accept non-sterile items.
- What are the regulatory requirements for this application? Some jurisdictions mandate sterility for products where others permit non-sterile. Always verify local regulations.
- What is the clinical consequence of potential contamination? High-consequence applications (neurosurgery, cardiac surgery) justify sterile supplies even where technically non-sterile might be acceptable.
- Can the facility ensure proper handling of non-sterile products? If staff training or protocols are inadequate, the safer choice is sterile products despite higher cost.
Special Considerations for Different Departments
Operating rooms should stock predominantly sterile supplies, with non-sterile items limited to skin preparation and patient positioning aids. Emergency departments benefit from both categories—sterile for wound repair and invasive procedures, non-sterile for examination and minor injury care. Outpatient clinics can often function effectively with primarily non-sterile supplies, reserving sterile items for specific procedures like joint injections or minor surgeries.
Packaging and Shelf Life Management
Sterile product packaging serves as a barrier system maintaining sterility until use. The most common materials include medical-grade paper-plastic pouches, Tyvek-plastic combinations, and multi-layer foil laminates. Each has specific permeability characteristics and sterility maintenance capabilities.
Package Integrity and Sterility Maintenance
Sterile package integrity depends on proper handling and storage. Packages should be inspected before use for tears, punctures, or moisture contamination—any compromise means the product should be considered non-sterile. We seal our sterile products using validated heat-seal parameters that create peelable seals withstanding 1.5-3.5 kg/cm pull force, ensuring integrity during shipping and handling while allowing easy aseptic opening.
Shelf life for sterile products isn't based on product degradation but on package integrity maintenance. Most sterile medical disposables carry 5-year shelf lives, after which the manufacturer can no longer guarantee the sterile barrier system remains intact. Non-sterile products typically have longer shelf lives or no expiration date, as their functionality depends on material properties rather than maintained sterility.
Storage Environment Requirements
Optimal storage for sterile products maintains 40-70% relative humidity and 20-25°C temperature. Higher humidity can compromise paper-based packaging materials, while lower humidity increases static electricity that may damage packaging during handling. Non-sterile products tolerate wider environmental variations, though extreme conditions can affect material properties—heat may affect elastic bandage stretch characteristics, and moisture can compact cotton products.
Quality Verification and Supplier Selection
When procuring sterile products, verification of sterilization validation is essential. Reputable manufacturers provide sterilization certificates including process parameters, biological indicator results, and lot-specific documentation. Our quality system maintains complete traceability from raw material through sterilization to final packaging, with annual re-validation of all sterilization processes.
Critical Quality Indicators
- ISO 13485 certification demonstrates a quality management system specific to medical devices, essential for both sterile and non-sterile manufacturers.
- Sterilization validation reports should document biological indicator performance, package integrity testing, and residual EtO levels (if applicable, must be below 10 ppm for EtO-sterilized products).
- Routine sterility testing using pharmacopeial methods (USP <71>, EP 2.6.1) on random samples from each sterilization batch provides ongoing verification.
- Package seal integrity testing through dye penetration or microbial challenge tests ensures the sterile barrier performs as intended.
For non-sterile products, verify that bioburden controls are in place. While not sterile, these products should still meet cleanliness standards appropriate for their intended use. Suppliers should provide bioburden data upon request, typically showing levels below 100 CFU per product or 1,000 CFU per gram of material.
Red Flags in Supplier Evaluation
Be cautious of suppliers offering suspiciously low prices for sterile products—proper sterilization and validation represent significant costs that cannot be eliminated without compromising quality. Inability to provide sterilization documentation, vague descriptions of sterilization methods, or reluctance to allow facility audits all suggest inadequate quality systems. We maintain open-door policies for customer audits and regularly host regulatory authority inspections at our Suzhou facility.
Practical Implementation in Healthcare Settings
Successfully managing sterile and non-sterile inventory requires clear protocols and staff education. We recommend implementing visual differentiation systems—sterile products stored in designated areas with clear signage, color-coded shelving, or dedicated supply carts. This prevents accidental substitution of non-sterile for sterile items during high-stress situations.
Staff Training Essentials
Clinical staff should understand not just which products are sterile, but why sterility matters for specific applications. Training should cover proper package opening techniques (peel pouches opened from the designated corner, maintaining sterile presentation), sterile field maintenance, and recognition of compromised packages. For non-sterile products, emphasize appropriate applications and the limitations—staff should understand that "non-sterile" doesn't mean "dirty" but rather "not guaranteed free of viable organisms."
Inventory Optimization Strategies
Many hospitals maintain excessive sterile inventory based on "just in case" mentality. Data-driven inventory management reveals that 80% of sterile product usage comes from scheduled procedures with predictable demand. By analyzing actual usage patterns, facilities can reduce sterile inventory carrying costs while maintaining appropriate stock for emergency situations. Non-sterile items, being more economical and longer-lasting, can support larger safety stocks without significant capital impact.
Implementing par-level systems with automatic reorder points prevents both overstocking and stockouts. For sterile items with 5-year shelf lives, maintaining 6-12 month supply levels balances availability against expiration risk. Non-sterile products tolerate 12-18 month supply levels more comfortably.
Making the Right Choice for Your Facility
The sterile versus non-sterile decision ultimately balances patient safety, clinical necessity, regulatory compliance, and economic reality. There are no universal answers—a product that must be sterile in one application may function perfectly well as non-sterile in another context. The key is developing institutional knowledge about which applications genuinely require sterility and which represent opportunities for cost-effective alternatives.
From our perspective as manufacturers serving diverse healthcare markets globally, we've seen successful facilities share common characteristics: clear protocols defining sterility requirements by procedure type, robust staff training emphasizing the rationale behind sterility choices, and strong supplier partnerships ensuring consistent quality whether products are sterile or non-sterile. These facilities achieve optimal patient outcomes while managing supply costs effectively.
When evaluating your facility's needs, consider conducting a product-by-product review using the risk assessment framework outlined above. You may discover opportunities to shift appropriate applications to non-sterile alternatives, freeing budget for enhanced sterile products in critical applications. Alternatively, you might identify gaps where current non-sterile product use poses unnecessary infection risks.
The medical disposables industry continues evolving, with innovations in sterilization technology, packaging materials, and quality control processes improving both sterile and non-sterile product options. Staying informed about these developments and maintaining open dialogue with qualified suppliers ensures your facility benefits from the latest advances while making evidence-based sterility decisions.

 English
English Français
Français Español
Español Português
Português عربى
عربى